When is the best time in cycle to test hormones? For menstrual cycle health checks, testing Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH) is best done on Day 3 of your period. Other hormones, like Progesterone, need testing just before your next period starts (around Day 21). We will walk through the timing for every key hormone test you might need.
Have you ever felt confused staring at a lab order, wondering exactly when you should take that blood test? It’s quite common! Getting the timing wrong when checking your hormones can completely throw off the results, making it feel like you’re back at square one. This isn’t like checking your engine oil; hormone levels shift dramatically every day. But don’t worry! We are going to break this down simply. Think of me as your trusted shop guide, showing you the exact sweet spot on your maintenance schedule for the best data. By selecting the right day, you ensure your doctor gets a clear, accurate picture of your body’s operations. Let’s unlock the right schedule so you can stop guessing and start understanding your results.
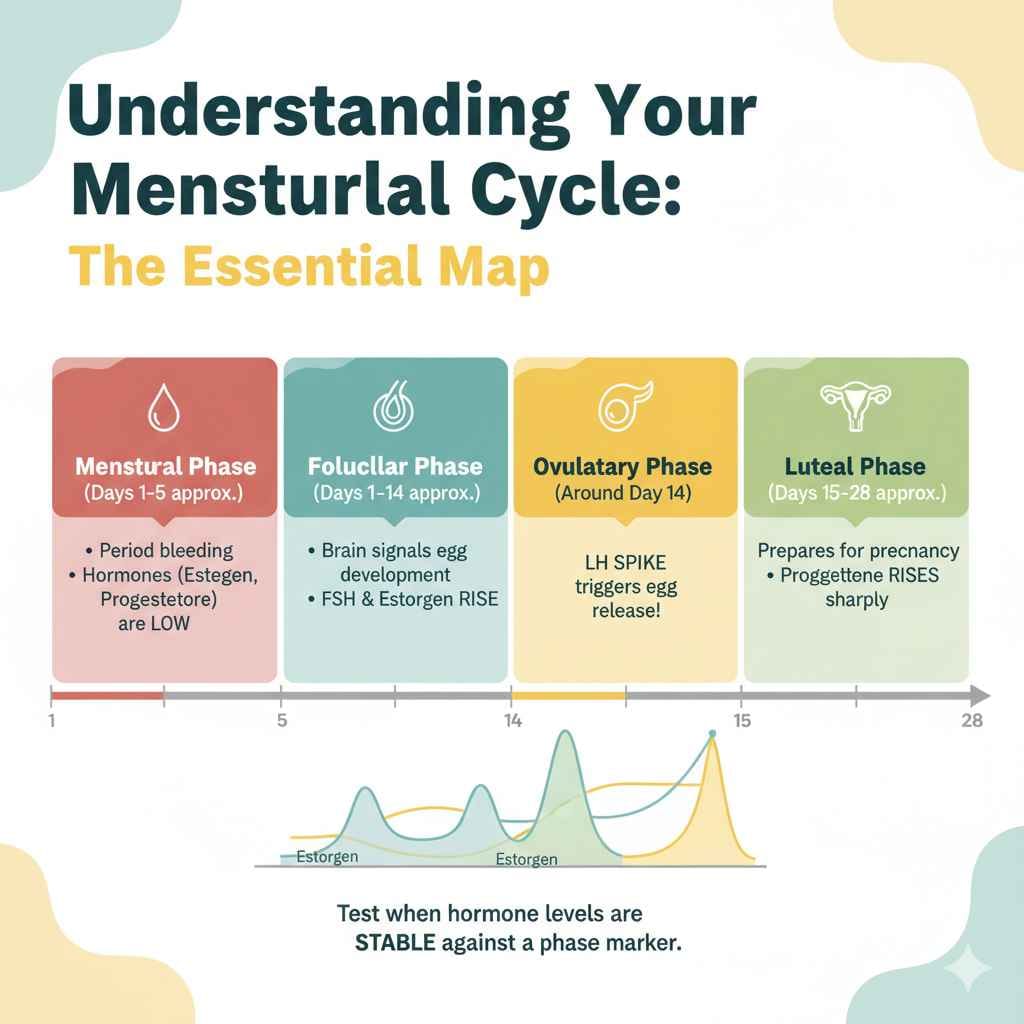
Understanding Your Menstrual Cycle: The Essential Map
Before we talk about when to test, we need a map. Your menstrual cycle is not one big block of time; it has distinct “zones” where hormone levels swing high or low. Knowing these zones helps us pinpoint the perfect moment for testing.
A typical cycle runs about 28 days, but anywhere from 21 to 35 days is considered normal. We measure “Day 1” as the first full day of your period bleeding.
There are four main phases, much like the four main checkpoints on a service route:
- Menstrual Phase (Days 1–5 approx.): This is when your period is happening. Shedding the uterine lining means hormone levels (like estrogen and progesterone) are low.
- Follicular Phase (Days 1–14 approx.): This phase starts on Day 1 and goes until ovulation. Your brain starts signaling for eggs to develop, raising FSH and then Estrogen levels.
- Ovulatory Phase (Around Day 14): This is the big event! A huge spike in LH triggers the release of an egg.
- Luteal Phase (Days 15–28 approx.): After ovulation, the body prepares for a possible pregnancy. Progesterone levels rise sharply here.
If you need consistent, reliable information, you need to test when hormone levels are stable against a specific phase marker—not during a rapid surge or crash.
The Quick Start Guide: Hormone Testing Cheat Sheet
If you need to check a few key players, here is the simplest schedule to remember. Keep this handy; it’s like the essential tool list you keep in your glove box.
| Hormone to Test | Best Time in Cycle to Test | Why This Timing Works |
|---|---|---|
| FSH (Follicle-Stimulating Hormone) | Day 2, 3, or 4 | Levels are lower and more stable before estrogen starts rising rapidly. |
| LH (Luteinizing Hormone) | Day 2, 3, or 4 | Testing early helps establish a baseline before the mid-cycle surge. |
| Estradiol (Primary Estrogen) | Day 2 or 3 | Checking levels when they are naturally low before the main follicular rise. |
| Progesterone | Day 20–22 (Mid-Luteal Phase) | Must be tested 5–7 days after ovulation to confirm if ovulation occurred. |
| Total Testosterone | Any day (Morning preferred) | Less cycle-dependent, but morning tests reflect normal morning peak levels. |
| Thyroid Hormones (TSH, Free T3/T4) | Any day (Fasting helps) | These are usually checked independent of the menstrual phase, but consistency matters. |
Detailed Breakdown: Timing for Specific Hormone Tests
Let’s look closely at why specific days matter for the most commonly requested hormone panels. Getting this right is crucial for accurate diagnosis, whether you are checking fertility, thyroid function, or approaching perimenopause.
Testing FSH and LH: Establishing a Baseline
Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH) are critical regulators released by your pituitary gland. They tell your ovaries what to do.
The Rule: Test early in the Follicular Phase (Days 2, 3, or 4).
Why not later? During the first few days of your period, your estrogen levels are naturally at their lowest point for the month. When estrogen is low, FSH and LH are easier to measure accurately. If you wait until Day 7 or 8, estrogen starts climbing, which can artificially suppress the FSH reading, making your ovarian reserve look potentially different than it actually is.
For fertility assessments or checking ovarian reserve, an early test gives the most consistent baseline data doctors rely on.
Testing Estradiol (Estrogen): Two Views
Estradiol (the main form of estrogen) fluctuates wildly throughout the month. Depending on what your doctor is looking for, you might test it at two very different times.
1. Baseline Estradiol (Day 3)
If you are checking your overall ovarian output or baseline function, Day 3 testing alongside FSH is necessary. Low Day 3 Estrogen usually suggests a healthy ovarian response is about to start.
2. Mid-Follicular Estradiol Peak (Around Day 10–13)
If the goal is to see how well your body is building up the uterine lining before ovulation, doctors sometimes test Estradiol right before the expected LH surge. This shows you if you have a strong follicular phase, which is essential for thickening the lining that a fertilized egg needs.
Testing Progesterone: Confirming Ovulation
Progesterone is crucial because it’s exclusively produced after ovulation (by the corpus luteum). Testing it too early won’t tell you anything useful about whether you ovulated that month.
The Rule: Test 5 to 7 days after you expect ovulation, or around Day 21 of a standard 28-day cycle.
If your cycle is irregular, use ovulation tracking methods (like clear, consistent basal body temperature charting, or ovulation predictor kits) to pinpoint ovulation. Once you know the day of ovulation, count six days forward.
If Progesterone is high (generally above 3.0 ng/mL, but labs differ) on this day, it strongly suggests ovulation successfully occurred.
If it’s low, it might indicate an anovulatory cycle (no egg released) or a Luteal Phase Defect (the body didn’t support the corpus luteum long enough).
This is a core test for tracking cycle health and investigating causes of infertility or irregular spotting.
Testing Total and Free Testosterone
Testosterone levels fluctuate much less dramatically day-to-day compared to estrogen or progesterone. While some minor fluctuations exist, it is less critical to nail the exact cycle day.
The Rule: Test in the morning (usually between 8:00 AM and 10:00 AM), anytime during the follicular phase (Days 3–10).
Why the morning? Like many hormones, testosterone hits its natural peak early in the day. Testing in the morning ensures you catch this peak, giving you reliable readings for assessing conditions like Polycystic Ovary Syndrome (PCOS) or general energy levels.
Testing Thyroid Hormones (TSH, Free T3, Free T4)
Thyroid stimulating hormone (TSH) and the active thyroid hormones are generally not affected by the menstrual cycle phases. However, consistency is key for good readings.
The Rule: Test on an empty stomach, ideally first thing in the morning, regardless of cycle day.
If you are taking synthetic thyroid replacement medication (like Levothyroxine), the testing protocol is very strict: you usually need to fast and skip your morning dose on the day of the blood draw. Always confirm this specific protocol with your ordering physician or the actual lab facility. For reliable results, it helps to keep feeding times and stress levels consistent across tests, as these factors influence TSH.
Navigating Irregular Cycles: When You Can’t Rely on Day Numbers
What if your cycle is wildly unpredictable, or you haven’t had a period in months (amenorrhea)? Relying on “Day 3” or “Day 21” becomes impossible. In these situations, doctors switch gears.
Testing During Bleeding (Regardless of Day Count)
If you are bleeding, but it’s not a typical period bleed (perhaps spotting or very light flow), Day 3 testing still often works for FSH/LH baseline checks, provided the bleeding is consistently light and doesn’t resemble a full withdrawal bleed. For the most accurate baseline, however, doctors often prefer to wait until true bleeding starts or sometimes recommend a “Reset” period without treatment to try and induce a normal cycle start.
Testing for PCOS or High Androgens
If the primary concern is high androgens (like testosterone), the cycle day is less critical than the time of day. You mainly need to test when symptoms are present or in the morning for the most reliable androgen assessment. Sometimes, testing twice—early follicular phase AND mid-luteal phase—is done to compare how estrogen/progesterone are interacting with the androgens.
Special Consideration: Testing After Menopause or Perimenopause
Once you are consistently post-menopausal, the standard cycle testing rules no longer apply, as the cyclical surges stop. However, during perimenopause (the transition years), testing becomes tricky because hormone levels swing wildly.
In perimenopause, doctors often must test FSH multiple times (sometimes weeks apart) because a low reading might just mean you hit a temporary high estrogen point. High, consistently rising FSH levels often confirm the shift into menopause, as the ovaries are struggling to respond.
Practical Steps: Preparing for Your Hormone Blood Draw
Just like preparing your car for an oil change involves having the right filters and oil grade, preparing your body for a blood draw ensures the results are usable right off the service ramp.
Essential Preparation Steps Before the Draw:
- Confirm the Date: Always double-check the exact day number with your healthcare provider. If they say Day 3, count your first day of heavy flow as Day 1.
- Fasting (If Required): Check if your lab requires fasting (no food or caloric drinks) for any specific tests (like cholesterol markers often grouped with hormone panels). Thyroid tests often require strict fasting protocols.
- Medication Review: Never stop prescribed medications without talking to your doctor. However, tell the nurse or phlebotomist everything you are taking, especially birth control pills or hormone supplements, as these can completely mask your natural hormone levels.
- Hydration and Rest: Be well-hydrated (it makes finding veins easier!) and try to rest well the night before. High stress can elevate cortisol, which impacts other hormone outputs.
- Time of Day Matters: Morning draws (before 10 AM) are standard for most basal hormone checks (FSH, LH, Testosterone) because of natural morning peaks. Progesterone testing schedule needs to align with ovulation, not just morning timing.
Tools to Help You Track Your Cycle Accurately
Accurate tracking is half the battle. If you are manually tracking, you need reliable instruments. For example, understanding basal body temperature (BBT) helps pinpoint when the Progesterone shift occurred.
- Fertility Apps/Journals: Use dedicated apps or detailed paper journals to log bleeding, spotting, cervical mucus changes, and temperature readings consistently.
- Basal Thermometer: A special thermometer that measures tiny temperature shifts (to the hundredth of a degree) is essential for confirming ovulation via BBT shift. You can find reliable models from various reputable health technology manufacturers.
- Ovulation Predictor Kits (OPKs): These urine strips measure the LH surge, giving you an early warning that Day 21 testing for progesterone is coming up in about a week.
For more on understanding these tracking methods, organizations like the Centers for Disease Control and Prevention (CDC) offer great resources on reproductive health basics, which can help standardize your tracking methods.
Hormone Interaction: Why Timing Affects Diagnosis
Imagine your hormones are like the different teams working on an engine. If one team (like Estrogen) is scheduled for maintenance, you don’t want to check the performance of the other team (like FSH) while they are supposed to be resting.
Hormones work in a feedback loop. This is similar to how your car’s computer system works: an input affects the output.
If you test FSH on Day 10 when Estrogen is peaking, the high Estrogen tells the pituitary gland to stop releasing FSH. The lab result will show temporarily low FSH, leading to a potential misdiagnosis that your ovarian reserve is better than it truly is when tested correctly on Day 3.
Conversely, testing Progesterone on Day 5 will yield zero useful data, as the primary source of Progesterone (the follicle that released the egg) hasn’t even formed yet.
This interdependence is why the strict timing rules exist; they strip away the normal fluctuations so the doctor can see the underlying baseline function of the glands involved.
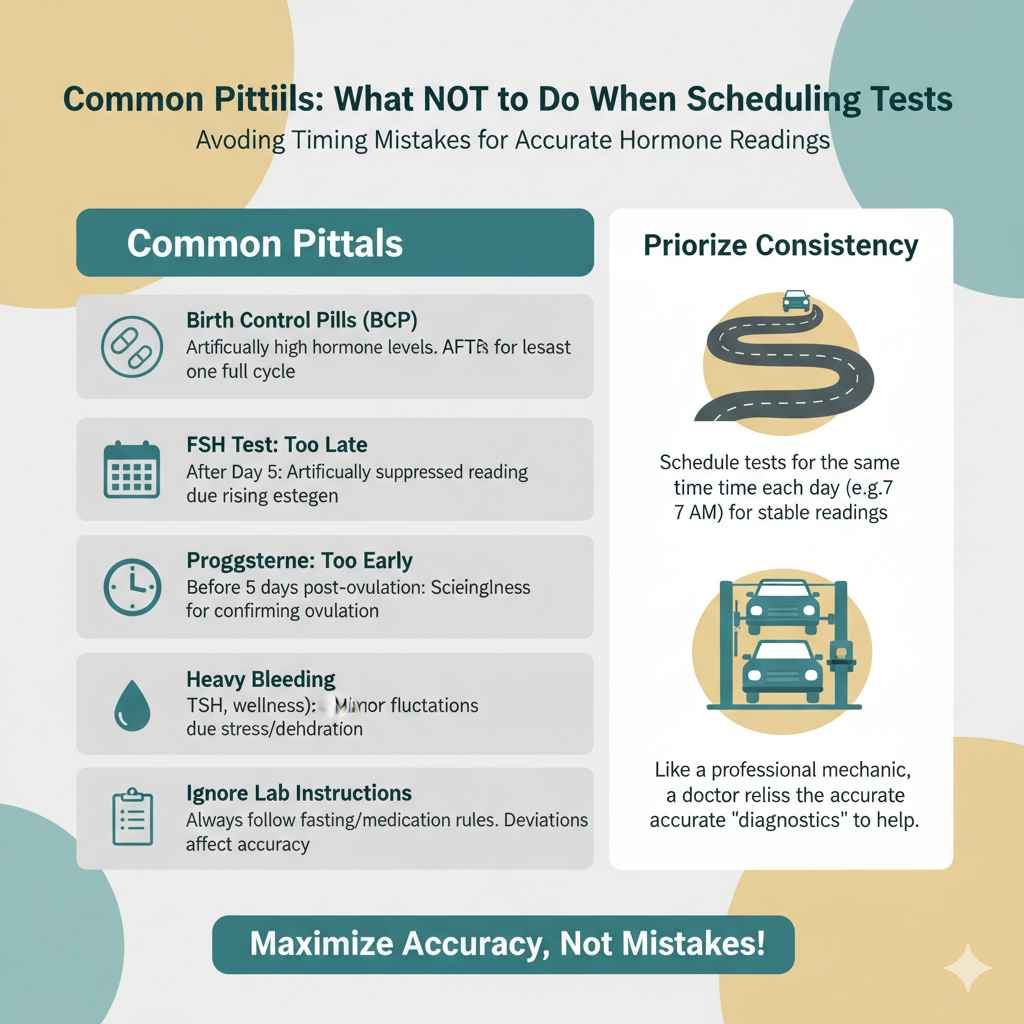
Common Pitfalls: What NOT to Do When Scheduling Tests
Even with the best intentions, drivers sometimes take a wrong turn. Here are the most common timing mistakes people make when trying to test hormones.
- Taking the Test While on Birth Control Pills (BCP): Most hormonal contraceptives—oral pills, patches, or rings—artificially keep your estrogen and progesterone levels steady and high. Testing while on BCPs provides information about the medication’s effects, NOT your natural biological cycle. If seeking fertility or cycle insight, the BCPs must usually be stopped for at least one full cycle before testing.
- Testing Too Late in the Follicular Phase for Baseline: As mentioned, testing FSH after Day 5 often results in an artificially suppressed reading due to rising estradiol.
- Testing Progesterone Too Early: Any result before 5 days post-ovulation is scientifically meaningless for confirming ovulation.
- Testing During Heavy Bleeding for Non-Menstrual Tests: While Day 3 is for baseline, testing TSH or general wellness markers during the heavy flow might sometimes cause minor fluctuations due to acute stress or dehydration. Stick to the morning baseline rule for those.
- Ignoring Lab Instructions: If the lab specifies you must fast, or you must test before taking your morning medication—follow their instruction precisely. Deviating is like driving a modern car without correcting for tire pressure—it affects the overall performance reading.
To ensure you are getting accurate readings, always prioritize consistency. If you normally wake up at 7 AM, try to schedule your appointment around the same time each cycle day you test, as cortisol levels naturally drop throughout the morning.
FAQs: Beginner Questions About Hormone Testing Timing
Here are some quick answers to common questions people have when first navigating the world of cycle-specific blood draws.
Q1: If I have a 35-day cycle, what day should I test FSH?
A: Even with a longer cycle, the goal for baseline FSH is to test early, before estrogen starts rising significantly. Aim for around Day 3, Day 4, or Day 5. Your doctor may advise you to test slightly later, like Day 5 or 6, to account for the longer follicular phase, but Day 3 testing remains the standard starting point.
Q2: Can I use an ovulation test strip instead of a blood test for Progesterone?
A: No, ovulation strips only test for the LH surge, which happens 24–36 hours before ovulation. They cannot substitute for a blood test used to measure the actual Progesterone level produced after ovulation. Blood testing is required to confirm luteal phase function.
Q3: What happens if I forget my period start date and can’t do Day 3 testing?
A: If you miss the Day 3 window, it’s best to contact your physician. In many cases, they will still order the test, but they will mark the results as “non-baseline” or may ask you to repeat the FSH/LH test in the next cycle when you can track the start date accurately.
Q4: Do I need to stop exercising or drinking caffeine before my hormone tests?
A: For standard cycle timing tests (FSH, LH, Progesterone), moderate exercise and normal caffeine intake usually won’t drastically skew the results, especially compared to the powerful effect of diet on glucose or lipid panels. However, extreme exercise or high stress on the day of the test should be avoided, as high cortisol can influence other hormones.
Q5: If I am trying to get pregnant, does the timing change for every hormone?
A: Yes. For fertility workups, you generally need two specific windows: an early window (Day 3 for FSH/Estrogen baseline) and a mid-luteal window (Day 21 for Progesterone confirmation). Testosterone and Thyroid checks are more flexible but should still be done consistently.
Q6: Is testing hormones at home the same as a lab test regarding timing?
A: Home urine testing kits are great for LH surges but are not reliable for quantitative testing of hormones like FSH or Progesterone in the way a lab blood draw is. For complex cycle diagnosis, always trust the timing protocols given for venous blood draws.
Conclusion: Driving Confidently with the Right Schedule
Hormone testing is only accurate when it’s done at the right time in your menstrual cycle. Early-cycle testing (Days 2–4) gives a true baseline for hormones like FSH, LH, and estrogen, while mid-luteal testing (about 5–7 days after ovulation) is essential for progesterone. Other hormones, such as thyroid markers and testosterone, are less cycle-dependent but still benefit from consistent morning testing.
By matching each hormone test to the correct cycle phase—and preparing properly—you ensure results that actually reflect how your body is functioning. Correct timing removes confusion, prevents misdiagnosis, and gives both you and your doctor clear, actionable information instead of misleading numbers.

