The best time to start most types of combined hormonal birth control (pills, patch, ring) is the first day of your period. This ensures immediate protection against pregnancy. For the mini-pill, you can often start any day, but timing rules vary slightly for all methods, so always check the specific instructions.
Learning about your menstrual cycle can feel a bit like reading an old car maintenance manual—full of terms that sound complicated! Many people feel unsure about starting a new birth control method. Which day is right? Will it work right away? Getting this timing wrong can cause unnecessary worry or mean you need extra backup protection. Don’t stress! We are going to break down the timing secrets for starting birth control so you can feel confident and safe. This guide will explain exactly when to pop that first pill or apply that first patch, based on what works best for your body. Think of this as getting your personalized start-up checklist.
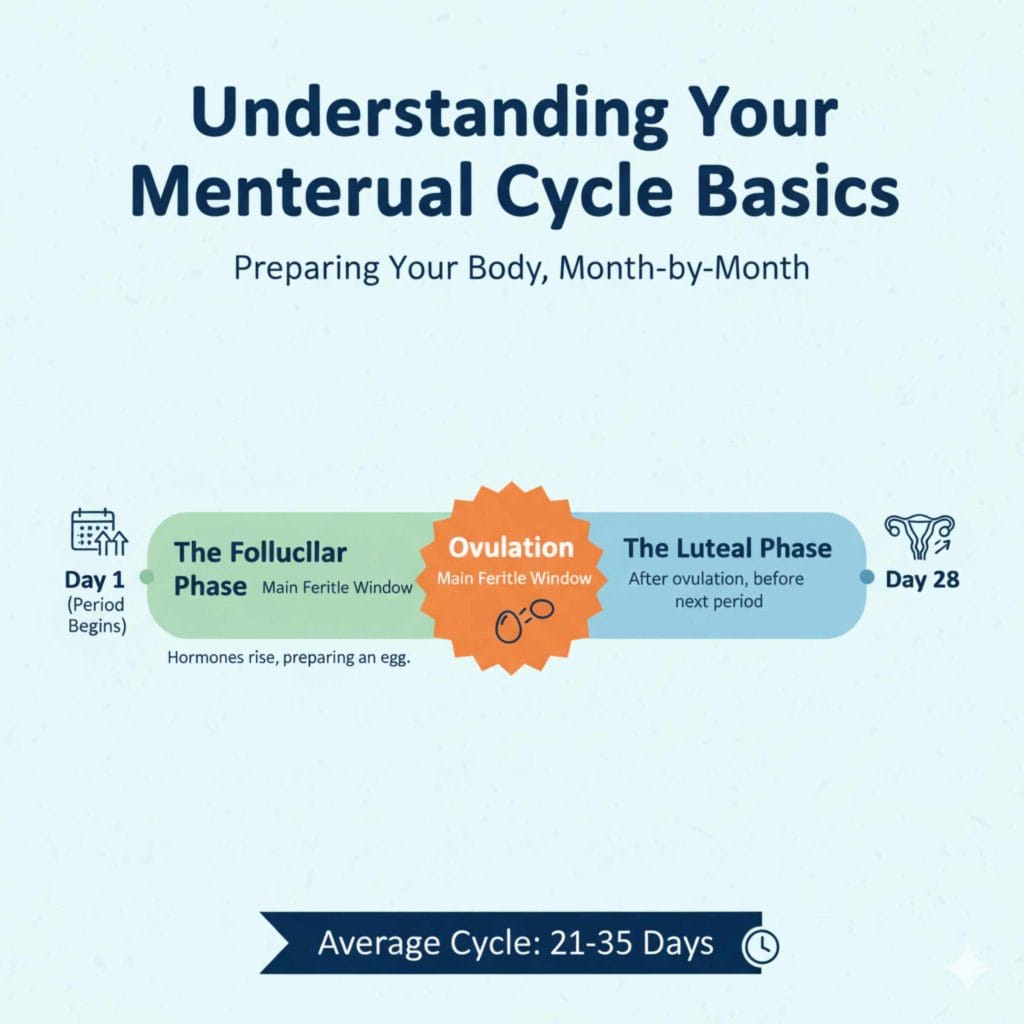
Understanding Your Menstrual Cycle Basics
Before we dive into the starting times, let’s quickly look at what’s happening in your body. Your menstrual cycle is basically a monthly process preparing your body for pregnancy. It usually lasts about 28 days, but anything from 21 to 35 days is normal.
The cycle has a few key phases:
- The Follicular Phase: This phase starts on Day 1 of your period and lasts until ovulation. Hormones are slowly rising.
- Ovulation: This is when an egg is released from the ovary. This is the main fertile window.
- The Luteal Phase: This phase happens after ovulation and before your next period starts.
Knowing where you are in this cycle helps explain why certain starting times are recommended for different birth control methods. Think of it like knowing if your engine is cold or warm before you start driving hard.
The Big Question: When Is The Best Time To Start Birth Control?
The answer depends heavily on the type of birth control you are using. Different methods have different rules regarding immediate effectiveness and preventing ovulation right away. We will focus on the most common methods used by beginners.
Combined Hormonal Contraceptives (Pill, Patch, Ring)
Combined methods use both estrogen and progestin. These are the most common types where timing matters most for immediate protection.
Option 1: The Quick Start Method (Often Recommended)
The “Quick Start” method is very popular because it’s easy to remember and offers near-immediate protection if you follow the rules perfectly.
With the Quick Start method, you begin taking your pill (or applying your patch/inserting your ring) on the very first day you start bleeding (Day 1 of your period).
Why this is great:
- You know for sure you are not pregnant when you start.
- Protection is immediate. You usually do not need backup birth control (like condoms) when first starting.
- It simplifies remembering—just start when your period shows up.
Option 2: The Sunday Start Rule (For Scheduling Ease)
Some people prefer to have their withdrawal bleeding (the placebo week) fall on a convenient time—often starting on a Sunday.
If you choose the Sunday start, you begin the pill pack on the Sunday following the start of your period.
Important Note on Sunday Start: If you start on a Sunday, but your period did not start until Tuesday or Wednesday, you might not be protected right away. In this case, you must use a backup method for the first seven days you take the pill. This is why “Quick Start” is often safer for immediate protection.
Progestin-Only Methods (The Mini-Pill)
The mini-pill works a bit differently because it only uses progestin. Because it works mainly by thickening cervical mucus, the timing rules are less strict, but precision is still key.
For most mini-pills:
- You can usually start any day of your cycle, even if you are bleeding.
- The key is consistency. You must take the mini-pill at the exact same time every day.
However, if you are starting the mini-pill more than 3 days after you stopped your last period, or if you haven’t had a period, your doctor may advise using backup protection for the first 48 hours. Always confirm with your healthcare provider, as some older mini-pills have stricter rules.
Long-Acting Reversible Contraceptives (LARCs)
LARCs include options like the hormonal IUD (like Mirena or Skyla) or the implant (like Nexplanon). These are often called “set-it-and-forget-it” methods because they offer protection for years.
For LARCs, the timing is highly flexible:
- Provider’s Office Start: If you have a LARC inserted during a doctor’s visit, it is effective immediately if inserted within the first 5 days of your normal period.
- Flexible Start: If the provider inserts it at any other time (or if you aren’t sure if you’re pregnant), they will often advise using backup protection for 7 days after insertion.
LARCs aim to stop ovulation altogether, so the timing guidelines are mostly about ruling out pregnancy at the insertion moment.
Side-by-Side Comparison of Starting Methods
To make this crystal clear, let’s look at the methods side-by-side. Remember, always follow the specific instructions provided by the manufacturer or your doctor, but this is a helpful overview.
| Birth Control Type | Best Time to Start (For Immediate Protection) | Backup Needed? |
|---|---|---|
| Combined Pill, Patch, Ring (Quick Start) | Day 1 of your period. | Generally NO backup needed if you start on Day 1. |
| Combined Pill (Sunday Start) | The Sunday after your period begins. | YES, use backup for the first 7 days. |
| Mini-Pill (Progestin-Only) | Any day, but must be taken at the same time daily. | Possibly backup for 48 hours if started outside the first few days of your period. |
| Hormonal IUD/Implant (LARC) | If inserted within the first 5 days of bleeding. | YES, use backup for 7 days if inserted outside that 5-day window. |
The “What If” Scenarios: Starting When You Are Not on Your Period
This is where people often get confused or nervous. What if you just want to start today, but your period isn’t due for another week? This is called starting “outside the window.”
Starting Combined Pills When You Aren’t Bleeding
If you decide to start your combined pill pack on a random day of the month (not Day 1 of your period), you are using the Quick Start method, but with a precaution, because there is a small chance you might already be ovulating or have just ovulated.
The Rule: If you start taking the combined pill on any day other than Day 1 of your period, you MUST use a barrier method (like condoms) for the first full 7 days.
During those initial 7 days, the hormones need time to build up in your system to effectively stop you from releasing an egg. If you have unprotected sex during those first 7 days, there is a risk of pregnancy. This is why aligning the start with Day 1 is often the least stressful choice!
Starting Right After Stopping Another Method
Timing is often easier if you are switching methods.
Switching from another Combined Pill to a New One
If you are switching from one brand of combined pill to another, or even switching from the patch to the ring, your ability to switch directly is usually seamless.
You usually start the new method the very next day after stopping the old one, with no break. This prevents any gap in hormone coverage.
Switching From Hormonal Birth Control to the Mini-Pill
This switch requires a little more care because the mini-pill is less forgiving about timing.
- If you were using a combined pill, patch, or ring: Stop the old method and start the mini-pill the very next day. You won’t need backup protection if you take the mini-pill within 3 hours of when you would have taken your previous pill (or applied the patch/ring on schedule).
- If you were using an IUD or Implant: Remove the LARC and start the mini-pill the same day, or the next day at the latest. If you wait more than a day, use backup protection for the first 7 days of the mini-pill.
Why Immediate Protection Matters: Hormonal Mechanism
When you start birth control, the goal is to quickly establish enough hormone levels to prevent ovulation—releasing an egg.
When you use the “Quick Start” (Day 1 start), your body is naturally out of its most fertile window. The hormones immediately start to suppress the signals telling your ovaries to prepare an egg. Because the natural surge that causes ovulation hasn’t happened yet, the pill kicks in right away.
If you start in the middle of your cycle, there is a slight chance that the natural hormonal changes have already started the process of bringing an egg to maturity. The pill needs a few days to overcome that existing push. That’s why we use those 7 days of backup protection for safety.
This concept is similar to how you treat major vehicle maintenance; if you wait until the engine light is flashing brightly (peak fertility), fixing the underlying issue takes longer than if you catch a small issue early on (starting at Day 1).
For more detailed information on how different contraceptives work to prevent pregnancy, you can review resources from organizations like the Centers for Disease Control and Prevention (CDC) regarding contraceptive effectiveness and usage guidelines.
Keeping Track: Essential Records and Check-Ins
Once you start, the best time to continue taking the pill is the most important aspect for effectiveness. Consistency is king!
Tips for Remembering Your Daily Dose (Pills)
It can feel like a chore at first, similar to remembering to check your tire pressure every month. Here are ways to build that habit:
- Link It to an Existing Habit: Take your pill right after brushing your teeth at night or while eating breakfast the next morning.
- Set Phone Alarms: Use a recurring alarm labeled clearly, “Take the Pill!”
- Use a Tracking App: Many birth control apps exist that can send reminders and track your cycle days.
- Use the Calendar Pack: If your pill pack has days printed on it, use that visual cue to stay on track.
When to Contact Your Doctor After Starting
It’s normal to have some side effects as your body adjusts, such as spotting or mild nausea in the first month or two. However, if you experience certain things, or if your initial start time throws you off, it’s time to call your provider.
| Symptom | Action Required |
|---|---|
| Missed Period (While on combined pills) | Take a pregnancy test after missing the second period. |
| Severe Leg Pain or Shortness of Breath | Seek immediate medical attention (possible blood clot sign). |
| Spotting after 3 Months | Call your doctor for a check-in; may need a dosage adjustment. |
| Severe Headaches or Vision Changes | Contact your doctor promptly. |
A Deeper Look: Starting When You Are Not Sure About Your Last Period
This scenario comes up often, especially for people with irregular cycles or those who haven’t had a period in a while (like postpartum mothers or teens).
If You Have Irregular Cycles
If your cycle is unpredictable, using the “Sunday Start” is highly risky because you cannot guarantee you are on Day 1.
Recommendation: For irregular cycles, always opt for the Quick Start (start today, Day 1 of bleeding) or use the “Start Anytime + Backup” rule (start today, use condoms for 7 days).
If you have reached the point where you are starting birth control because you hope to regulate those cycles, starting immediately is the goal, backed up by condoms until the 7-day mark is hit.
If You Just Gave Birth (Postpartum)
The timing for starting birth control after delivery is crucial and varies widely based on whether you plan to breastfeed.
If you are not breastfeeding, you can usually start combined pills 3–6 weeks postpartum, sometimes sooner.
If you are breastfeeding, doctors often recommend waiting 6–8 weeks, or suggest using progestin-only methods (like the mini-pill or hormonal IUD) right away, as estrogen in combined methods can sometimes affect milk supply.
Always consult your obstetrician before starting any hormonal method postpartum, as pregnancy risk is high after delivery.
If You Just Had a Miscarriage or Abortion
Medical professionals recommend starting hormonal birth control immediately (within the first 24–72 hours) following a miscarriage or abortion, whenever possible. Starting right away minimizes the window where pregnancy could recur rapidly. In this situation, the timing is less about the menstrual cycle and more about rapid protection.
Comparing Hormonal Start Times vs. Non-Hormonal Methods
It is helpful to know that timing only applies strictly to hormonal contraception because those methods rely on immediately overriding your natural cycle hormones.
Non-hormonal methods do not rely on your cycle timing and offer immediate protection upon correct placement or use.
- Copper IUD: Effective immediately upon insertion, regardless of where you are in your cycle—as long as you are not already pregnant.
- Diaphragm/Cervical Cap: Must be used correctly every time you have sex, along with spermicide. Protection is immediate upon correct use.
- Spermicides/Condoms: Protection is immediate upon their correct first use.
If you are looking for immediate pregnancy protection starting today without worrying about Day 1, a visit to the clinic for a Copper IUD insertion might be the best route, followed by 7 days of abstinence or backup if you choose a hormonal pill standard start.
Building Confidence: Making the Switch
Switching birth control methods can feel daunting—like changing the spark plugs on a car without knowing what you’re doing. It feels risky. But remember, millions of people switch methods safely every year. The key is having a clear plan for that first week.
Three Steps to a Confident Start
1. Decide On Your Strategy: Will you wait for Day 1 (Quick Start) for guaranteed immediate protection, or will you start now and commit to backup protection for 7 days?
2. Schedule Your Backup: If you start outside of Day 1, immediately put a reminder in your phone or calendar for 7 days later. That date marks the day you can stop worrying about condoms.
3. Prepare Your Supplies: Have your pills, patch, or ring ready to go. If you are using condoms as backup, make sure you have a reliable supply on hand that isn’t expired.
Remember that your cycle is unique. If you are struggling to track your periods reliably—perhaps they are often late or very short—consider talking to your doctor about using an app or tracking Basal Body Temperature (BBT) for a cycle or two to confirm when Day 1 actually is before you start your method.
Frequently Asked Questions (FAQ) for Beginners
Q1: If I start my pill pack on a random Tuesday, why do I still need condoms for 7 days?
A: When you start mid-cycle, the hormones need about a week to fully suppress the surge that releases an egg (ovulation). Condoms protect you during that week the hormones are “warming up” to their full effectiveness.
Q2: What is the absolute safest time to start birth control to guarantee I am protected immediately?
A: The safest time for combined hormonal methods (pill, patch, ring) is the very first day you start bleeding—Day 1 of your period. No backup is typically needed then.
Q3: Can I start birth control if I think I might be pregnant already?
A: You should take a pregnancy test before starting any new hormonal birth control, especially if it has been more than 5 days since your last period ended, or if your period is late. Most methods are safe early in pregnancy, but it’s best practice to confirm you are not pregnant first.
Q4: If I start the mini-pill today, but I haven’t had a period in months, what should I do?
A: If you haven’t had a period and aren’t sure if you are pregnant, you should take a pregnancy test. If it’s negative, start the mini-pill today and use backup protection (like condoms) for the next 48 hours, as directed in the instructions.
Conclusion: Start Birth Control with Confidence, Not Confusion
The best time to start birth control depends on the method you choose—but for most hormonal options, starting on the first day of your period offers the simplest and safest path to immediate protection. When that timing isn’t possible, starting at another point in your cycle is still effective as long as you follow the backup rules carefully.
Understanding why timing matters—how hormones prevent ovulation and need time to take full effect—turns a stressful decision into a manageable plan. Whether you choose the pill, patch, ring, mini-pill, or a long-acting option, the key factors are timing, consistency, and using backup protection when needed.
Your cycle is unique, and there’s no one-size-fits-all answer. The good news is that with the right information—and a quick check-in with a healthcare provider when needed—you can start birth control safely, confidently, and on your terms.

